What’s This Research About?
Chronic pain needs to be treated differently than acute pain because there are different mechanisms at play. In a healthy system, acute pain is used as an alarm system, warning of possible threats to the body. For example, the alarm message of pain from your hand on a hot stove is sent to the brain so you move your hand and avoid burning it.
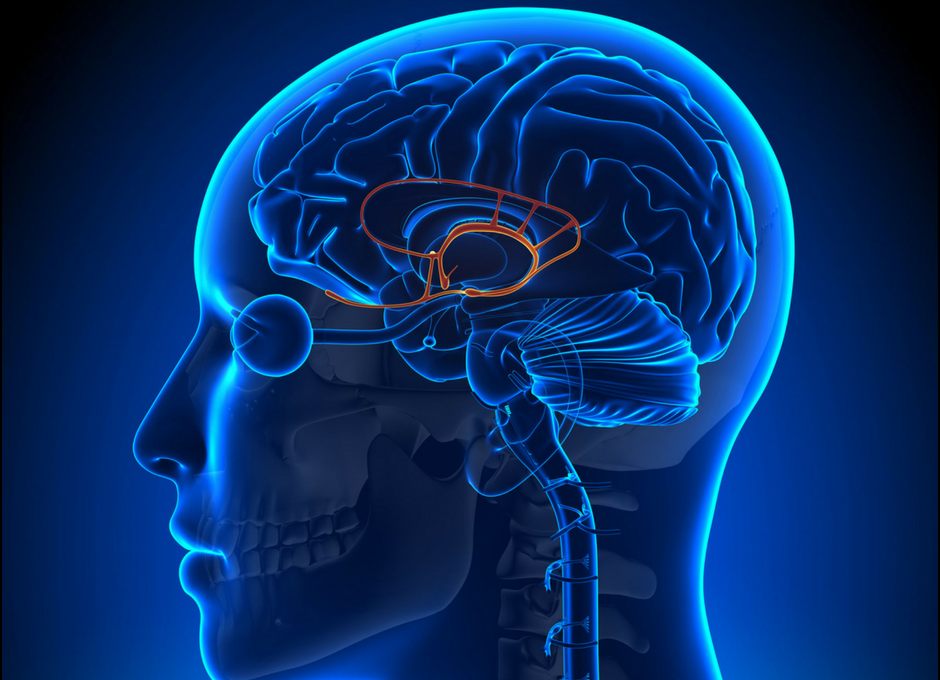
Chronic pain is more complicated and often involves a hyper arousal state of the nervous system which in turn can exacerbate symptoms. Pain messages are processed simultaneously with a lot more data than potential threats. This other data can come from the hand itself, the spinal cord, temperature, pH levels, stress hormones, or even the simple visual input of looking at the color red, which happens to increase pain sensitivity. The brain will ignore or amplify the message of pain by processing all of this incoming data. When it comes to chronic pain, the research suggests that the processor, the brain itself, can get high-jacked and can perpetuate the state of chronic pain without any actual impending threat of danger.
Chronic pain affects approximately 116 million people (much of our current opioid epidemic stems from the fact that opioids are still the treatment of choice). For the most part, the medical field still attempts to treat tissues locally with shots, surgeries, or pills to alleviate chronic pain. The researchers point out the focus should shift to the “brain emotional learning and memory circuitry” in order to create more effective treatments for chronic pain.
TITLE: Chronic Pain: The Role of Learning and Brain Plasticity
PUBLICATION: Restorative Neurology and Neuroscience
DATE: 2014
AUTHORS : A.R. Mansour, M.A. Farmer, M.N Baliki, A. Vania Apkarian
Associative learning: A concept in behavioral psychology that states a new response or learned behavior (i.e. fear of running) can be formed based on a particular stimulus (i.e. injury while running). Pain research shows high levels of fear can result in avoidance of pain and pain-related fear, which can lead to disuse, disability, and further pain.
Limbic system: Parts of the brain, such as the hypothalamus, amygdala, cingulate gyrus, hippocampus, and nucleus accumbens, located deep in the brain that are responsible for motivation, emotion, learning, and memory.

